Comprehensive Management of Back and Neck Pain CE25-478526, $169 9.5 CEUs
-
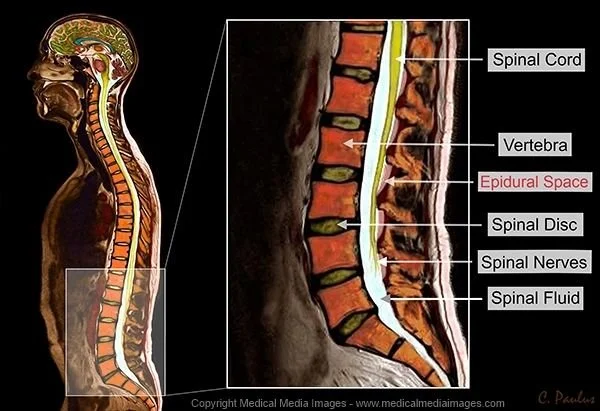
This seminar will provide a comprehensive review of current options for treating back and neck pain. Conservative treatments, including Physical Therapy, Manual Therapy, Pain Management, and Spinal Injections, will be explored by region.
The latest surgical techniques will also be covered, including Minimally Invasive Spine Surgery, Endoscopic Spine Surgery, Discectomy, Laminectomy, Spinal Fusion, Disc Replacement, Foraminotomy, and Scoliosis Surgery.
Additionally, spinal anatomy will be reviewed to support understanding of these treatments. Functional outcomes related to each treatment option will be discussed in detail.
This course now includes a 1-hour review of Stem Cell Therapy, currently used to treat certain spinal conditions. Emerging technologies such as Artificial Intelligence, Robotics, and related innovations will also be addressed.
Total Continuing Education Units (CEUs): 9.5
-
8:30-8:45 Course Objectives
8:45-9:00 History of management of back and neck pain
9:00-9:45 Future developments and projections and how these will affect our professions
9:45-10:00 Break
10:00-12:00 Spinal Anatomy
12:30-1:00 Lunch (on your own)
1:00-1:30 Common Dysfunctions
1:30-2:00 Compression Fractures
2:00-2:45 Spinal Stenosis
2:45-3:30 Disc Degeneration
3:30-3:45 Break
3:45-4:45 Spinal Implants
4:45-5:00 Spinal Injections/Importance of Education
5:00-5:15 Surgical Interventions
An Introduction to Manual Therapy for PT's and PTA's
CE25-1292577, $179 9.5 CEUs
-
There appears to be a misunderstanding or a disconnect among PTs and PTAs about what manual therapy consists of and how it should be used within our profession. This course will clear up this confusion by educating attendees on the current State Practice Acts and how these may affect the application of manual therapy.
We will define manual therapy and discuss its proper application and effect on the patient. A current review of the Chiropractic State Practice Act will be presented to facilitate discussion about the coexistence of Chiropractic and Physical Therapy.
Following this, attendees will learn about the development of manual therapy and the different perspectives that exist. This will include a discussion of theories brought forward by Evjenth, Kaltenborn, Paris, McKenzie, and others.
Before effectively applying manual therapy techniques, a solid understanding of anatomy, arthrology, and neurologic pathways is essential. These topics will be reviewed prior to a discussion on common joints that are mobilized.
Finally, the course will include a hands-on session demonstrating specific techniques, with an explanation of which techniques are appropriate for PTs and which are appropriate for PTAs.
Total Continuing Education Units (CEUs): 9.5
-
Practice Act Comparison: PT vs. PTA – Scope and Permissions
Understand the legal scope of practice for Physical Therapists (PTs) versus Physical Therapist Assistants (PTAs)
Clarify what tasks and interventions each professional is authorized to perform according to state practice acts
Highlight key differences and limitations to ensure compliance with regulations and optimal patient care
Chiropractic: A Legal Discussion
Overview of chiropractic practice within the context of manual therapy and rehabilitation
Examination of legal considerations and how chiropractic scope differs from PT and PTA practices
Joint Anatomy
Detailed review of joint structures, including bones, ligaments, capsules, and cartilage
Emphasis on anatomical features relevant to manual therapy interventions
Joint Physiology and Neuroanatomy
Exploration of the physiological functions of joints during movement
Understanding the neuroanatomical components influencing joint function and pain modulation
Arthrokinematics
Study of the small accessory motions occurring within joints during normal joint play
Application of arthrokinematic principles to assess and facilitate proper joint movement
Mobilizations: Different Views and Techniques
When to mobilize versus when to stabilize joints for optimal therapeutic outcomes
Overview of various mobilization approaches and their unique philosophies:
McKenzie Method
Kaltenborn Technique
Evjenth Approach
Paris Method
Maitland Concept
Mulligan Concept
Classifications of Mobilization
Distinguish between grades and types of mobilizations
Understand indications and goals for each classification to tailor treatments appropriately
Importance of Documentation
Emphasize thorough, accurate documentation for accountability and legal protection
Documentation best practices related to manual therapy interventions and progress tracking
Most Common Joints to Receive Mobilizations
Identify joints frequently targeted in manual therapy (e.g., cervical spine, lumbar spine, shoulder, knee, ankle)
Discuss typical pathologies and indications for mobilization in these joints
Practical Course Objectives
After attending this course, participants will:
Gain knowledge of the history and evolution of manual therapy
Understand differences in Practice Acts governing PTs, PTAs, and Chiropractors
Clearly define manual therapy and skilled passive range of motion
Appreciate arthrokinematics and effectively apply evidence-based mobilization techniques to facilitate joint movement
Differentiate among various classifications of mobilization and their appropriate clinical use
Recognize the critical importance of detailed and accurate documentation
Learn about the most common joints treated with mobilizations in clinical practice
New Technologies Affecting Post-Op Rehab
CE25-478524, $169 9.5 CEUs
-
With today’s rapid development and introduction of new orthopedic implants, it is challenging to keep pace with these advancements. This seminar will cover the latest developments in orthopedic replacement techniques and how these procedures impact postoperative rehabilitation. Topics include Genderknee, reverse shoulder, Birmingham hip resurfacing, and other emerging technologies.
The seminar will also address functional rehabilitation and its effect on clinical outcomes. This class has been updated to include discussions on Patient-Specific Cutting Blocks, navigation systems, and the latest hip and knee technologies, such as hip anteverted/retroverted systems and their influence on postoperative rehab.
Additionally, the introduction of AI technology into surgical practices will be explored.
Total Continuing Education Units (CEUs): 9.5
-
8:00–8:30 Registration
8:30–9:30 Objectives: Projected growth of elective orthopedic joint procedures and the effect this will have on our professions
9:30–11:30 Shoulder replacement surgeries
11:30–12:30 Elbow replacement
12:30–1:00 Lunch
1:00–2:00 Hip replacement procedures, including THA, partial, and Hip Resurfacing
2:00–3:00 Knee replacement procedures, including TKA, PKA, and Synvisc injection
3:00–4:00 Other important factors to consider, including Navigation, Custom Cutting Blocks, etc.
4:00–4:30 Importance of education and discharge planning
4:30–5:00 Review and Q&A
Clinical Imaging for the Rehab Specialist
CE25-815010, $169 9.5 CEUs
-
As the Physical Therapy profession advances toward becoming a first-line provider and Vision 2020 approaches, Physical Therapists are increasingly likely to see patients who have not been previously evaluated by a Medical Doctor. Additionally, with imaging technologies evolving at an accelerating pace, it is crucial for rehabilitation professionals to develop at least a basic understanding of the imaging options available today.
This course is designed for today’s rehabilitation professionals, including OT/OTA/PT/PTA, to provide an overview of current imaging modalities. It will also enhance attendees' understanding of why specific images are ordered, aiding in the development of more informed treatment plans.
Occupational Therapists and Occupational Therapy Assistants will particularly benefit from this seminar by gaining insight into the imaging studies their patients may undergo based on their diagnoses. Moreover, OT/OTA/PT/PTA participants will acquire a foundational understanding of the principles behind X-ray, CT, and MRI interpretations using the ABC acronym:
A for Alignment
B for Bone density
C for Cartilaginous (or Joint) space
By applying this acronym when reviewing images, clinicians will gain a better appreciation of the arthrokinematics contributing to patients’ symptoms. This understanding will enable more precise development and application of OT/PT plans of care.
The course will cover various joint disorders involving the shoulder, hand, fingers, wrist, knee, hip, ankle, and spine through the lens of the ABC approach.
Please note that this course does not train attendees to read images independently but emphasizes the relevance and application of contemporary imaging options in today’s rehabilitation practice. It is specifically designed for OT, OTA, PT, and PTA professionals.
Total Continuing Education Units (CEUs): 9.5
-
Understand why this class would be helpful to you as a healthcare provider.
Vision 2020: Position yourself as a first-line provider.
Address challenges in diagnosing effectively.
Recognize the importance of establishing the correct treatment diagnosis.
Develop skills to interpret imaging comprehensively:
Look beyond fractures to assess positioning, alignment, bone quality, muscle wasting, muscle imbalances, etc.
Utilize imaging as a patient educational tool.
Obtain a complete clinical picture without relying solely on others' interpretations.
Understand the legal aspects of imaging reports and their implications.
Gain knowledge of various imaging modalities, their history, and appropriate indications, including:
X-ray
CT/CAT
MRI
MRA
Myelogram
Fluoroscopy
Ultrasound
Nuclear Medicine
Bone scan
Others
Appreciate the clinical relevance of imaging and how it supports physical therapists (PTs) and physical therapist assistants (PTAs) in delivering accurate treatment diagnoses.
Differentiate between static and dynamic imaging techniques.
Review common fractures and pathologies encountered in practice.